Learn how SixthUp’s Payer Insights Solution helps a Pharmaceutical firm strengthen their commercial strategies with better coverage analysis, competitive intelligence and provider messaging on the access choices
Business Challenge
The pharma firm develops innovative oncology treatments for the US market. However, due to the emergence and the subsequent rise of biosimilar drugs, the firm is struggling with a dwindling market share.
There is an urgent need for deeper understanding of the evolving market dynamics, Payer preferences, sharpening Provider messaging and analyzing prescription behavior and competitive landscape along with a strong value proposition to the payers.

Few of the challenges that firm’s commercial and market access teams have to move past are as follows:
- Communicating value-based competitive advantage of the drug to Payers based on RWE (Real-world evidence)
- Analyze which of the payer contracts are working and which ones are not
- Deep dive into plans where competition has advantageous position over their product
- Providing compelling communication to Payers and Providers
- Determining the top drivers for rejection and the tactics that can be used to minimize the rejections
- Discovering ways to accelerate the growth of their brand
Firm needed a solution that could help them mitigate these challenges and enabled quick but also secure access to data that was typically siloed and in disparate systems.
After adequate due diligence, the firm selected SixthUp Payer Insights solution, which provides actionable insights with technology that connects RWE, payers, payer policies, open data and customer data.
Solution
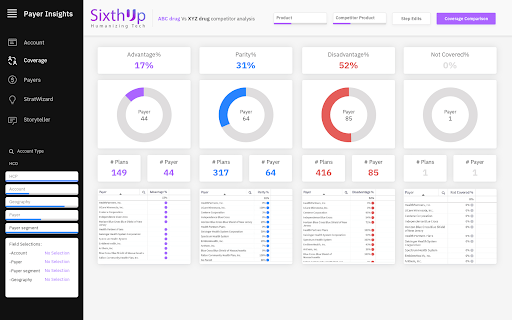
Sixth-up’s Payer Insights solution, is a robust, SaaS-based solution based on Cloud Data Lake architecture that connects internal data sources with real-world data to paint a complete picture of the commercial landscape, including payer/provider dynamics.
Key modules of the solution are:
- Payer Dashboards: Analysis and reporting on payer coverage, formulary status, competitive landscape with drill down to physician and geography level.
This helped the firm understand where they stand in comparison to competition, which contracts are really working and which ones need more focus, how payer formularies treat our product in coverage hierarchy as well as insights on the provider prescription behavior.
- Provider Messaging: Guidance on coverage messages for Providers to educate them about the access choices for the patients.
Sales and Market access teams are better prepared to answer any coverage questions for the providers. Digital and printed templates generated from the solution provide the coverage choices to the providers, further strengthening the messaging.
- Total Cost of Care Analysis: Risk stratification of the patient population and comparing total cost of care for each risk category with the competition to further provide value -based evidence for the payers. Robust risk stratification engine and TCOC model in the solution provides powerful insights on the patient population and payer positioning to the clients.
Impact

SixthUp’s solution enabled the pharma firm to get a thorough and sustainable grasp on the pharma competitive landscape, as well as the factors that influence payer purchase and provider prescription behaviors. It further helped them formulate a market access strategy as well as payer-provider marketing and brand strategies to mitigate their key business challenges. In summary, the firm’s commercial and market access teams were able to:
- Get Payer’s perspective of their product vs the competition.
- Enable rapid decision-making in payer contracting scenarios including granular step therapy analysis.
- Create a winning messaging strategy for their product geared towards health care providers, medical communities.
- Build future-forward commercial strategies and navigate access journey requirements.